Tracking your sleep and making sure you’re getting the most out of your rest seems like a harmless activity on the surface. However, the more sleep tracking wearables and smart mattresses available, the more people reporting increased stress and anxiety about achieving the perfect sleep — a condition called orthosomnia.
According to a 2023 survey by the American Academy of Sleep Medicine (AASM), around 1 in 3 US adults use sleep-tracking devices. Getting sleep data and tweaking your routine with the intention of improving your overall well being can be beneficial, until it goes too far.
But what does going too far look like? We asked the experts about what orthosomnia is, the common symptoms of it, and how to manage it so you can improve your sleep without inducing nighttime stress.
What is Orthosomnia?
The concept is easy to understand if we break down the term — ‘ortho’ means straight or correct while ‘somnia’ translates to sleep. Researchers coined this word as those who struggle with obsessing over achieving the correct or perfect sleep.
Although it sounds similar, orthosomnia is different from insomnia — a common sleep disorder. The former is not a clinically diagnosed disorder but rather a tendency to have an unhealthy preoccupation with your sleep data available through sleep trackers. Although, orthosomnia, if not managed, can lead to sleep issues including and not limited to insomnia.

Do sleep trackers cause orthosomnia?
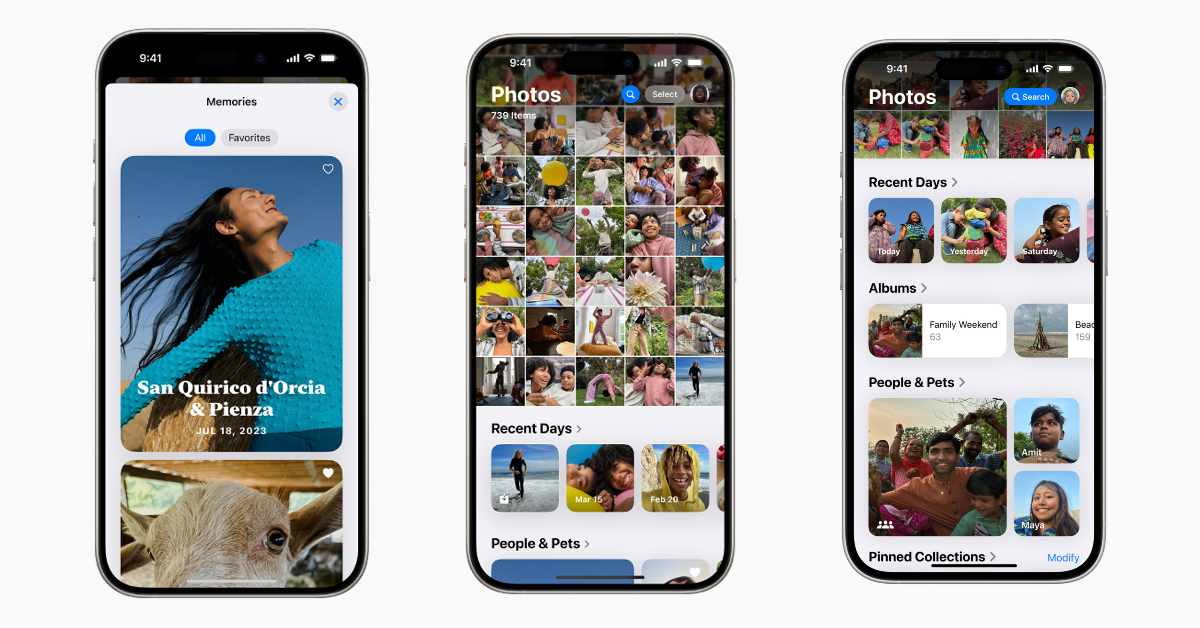
Recent studies reveal that the global wearable sleep trackers market is currently estimated to be 2.2 million USD and is expected to reach 3.29 billion by 2029. Tracking devices can improve your sleep by giving you important insights and information about your nighttime routines, but this can also be a gateway to obsession.
Most devices use accelerometers which measure how much you move in your sleep. In fact there are four main metrics sleep trackers monitor to analyze your sleep: movement, heart rates, respiration, and sound.
Fitbit, for instance, tracks your sleep stages by checking both your movement and heart rate. If you do not move for about an hour, the device assumes you’re sleeping and the length of time of your movements indicate your sleep behavior.

While trackers may claim to show details about specific sleep stages like REM sleep or deep sleep, these are not reliable. Basing it off on peripheral data like your movements or pulse rate has its limitations. It’s also important to keep in mind that it’s natural for the duration of the different sleep stages to differ as you get older and are in no way a signal of poor sleep. Trackers also cannot diagnose if you have particular sleep disorders like sleep apnea or insomnia, they can only detect patterns.
Overly tracking your ‘sleep performance’ can result in orthosomnia when you rely on these devices. You may tend to give more importance to the number of hours you slept rather than quality. In the long run, this can not only develop a mistrust in actual sleep science but will also lead you to self-diagnose yourself with certain conditions without consulting a medical expert.
The only way to get reliable facts about your sleep is to take part in a monitored sleep study by medical professionals.
What are some of the common symptoms of Orthosomnia?
Since it cannot be classified as a medical disorder yet, there are no official symptoms. The current discussions are based on case studies conducted by researchers and experiences people have shared on various platforms. Here are a few ways it can affect you:
You feel anxious at night
With orthosomnia comes nighttime anxiety about getting the best sleep possible, which often becomes counterproductive leading to disrupted sleep. If you find yourself feeling wide awake and stressed about sleeping exactly for 8 hours or getting perfect scores on your tracker, then you’re likely having sleep-related anxiety.
Studies have shown participants going through this “sleep paradox” when self-monitoring their habits goes overboard and actually induces stress which reaches its peak before bedtime. This is because your brain and body go into a state of ‘hyperarousal’ making it more difficult to quiet the mind which is focused on the end result of your sleep performance.

You rely on your sleep tracker
Dr Seema Khosla, a spokesperson of AASM (American Academy of Sleep Medicine) commented on how the growing popularity of sleep trackers are making people pay more attention to their sleep quality, routine and sleep duration.
Somewhere along the process, some sleepers are relying on the numbers you see on your tracker, which is where the problem starts. If you find yourself constantly thinking about your ‘sleep scores’ and how to do better every night, it might be a sign of orthosomnia.
You obsess over your sleep data
Checking and rechecking your sleep data may indicate an obsessive monitoring, especially if it causes stress. “People may feel frustrated or even exhausted by their sleep-tracking routines, trying to adjust bedtime habits in ways that ultimately make sleep feel more stressful," says Dr Michael Genovese, physician and chief medical advisor at Ascendant.
"Since the pandemic, we have seen a rise in orthosomnia cases as more people began tracking their health and sleep. While this awareness is often positive, for some, it has led to an unintended cycle of anxiety and restless nights,“ he continues.
How to manage Orthosomnia and get better sleep
Is it manageable? The short answer is, yes. However, it will require a lot of resolve to control the urge to track your sleep constantly. These are some ways you can navigate through:
Practice good sleep hygiene
Following good sleep hygiene habits is the key to falling asleep naturally. This means setting up the ideal environment for you to have a restful night’s sleep like a consistent sleep schedule, maintaining a clutter-free bedroom and sleeping on the best mattress for your sleep needs and best pillow to support your sleep position.
Drinking caffeinated beverages close to bedtime, using your bedroom for work or consuming too much sugary snacks on the other hand, will cause sleep disruptions.
Have a bedtime routine designed to reduce stress
It’s beneficial to remind your brain to winddown close to bedtime with a calming routine. You can start off with meditation techniques, breathing exercises or indulge in a nice warm shower.
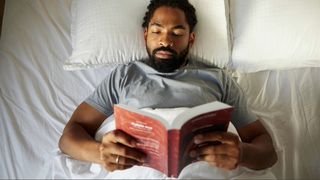
Taking up activities like reading or listening to gentle music can silence the noise in your head before sleep. Additionally reducing external distractions like sound pollution with a white noise machine and dimming the lights or using a blackout curtain can also do wonders.
Reduce screen time before bed
Exposing yourself to the bright light from your phone will suppress the production of melatonin, the sleep hormone. This can instead confuse the brain to be active, alert and overstimulated, adding to the stress and anxiety right before bed. Instead, opt for a book. This will help calm your mind and body before bed.
Cognitive Behavioural Therapy (CBT)
If you find that the symptoms of orthosomnia are persisting and affecting your day-to-day life or leading to sleep deprivation, CBT can tackle this issue. It is essentially a talking-therapy to gain control of your situation by focusing on your thoughts, feelings and actions. It is a pragmatic approach to improve your sleep administered by a sleep expert or certified medical practitioner.
“The key to managing orthosomnia is to reframe sleep goals so they’re based on how rested you feel rather than on-device scores. Cognitive-behavioral therapy for insomnia (CBT-I) is highly effective, helping people shift focus from numbers to developing a consistent, healthy sleep routine,” adds Dr Genovese.



















 English (US) ·
English (US) ·